 Treating Emphysema
Treating Emphysema
Although there is no cure for emphysema, appropriate management and treatment can reduce symptoms and improve your quality of life.
Medication
Depending on the severity of the disease, doctors use several kinds of medications to treat the symptoms and complications of emphysema. You may take some medications on a regular basis and others as needed.
These medications — which usually come in an inhaler form — open the airways in the lungs by relaxing the muscles around your airways. This can help relieve coughing and shortness of breath and make breathing easier. Depending on the severity of your disease, you may need a short-acting bronchodilator before activities, a long-acting bronchodilator that you use every day, or both.
Short-acting bronchodilators include inhalers to relieve symptoms like breathlessness and flare ups. A preventative measure is to use long-acting bronchodilators on a consistent basis to prevent these types of flare-ups occurring. They are seen as more long term therapies that keep symptoms of emphysema at bay.
Inhaled corticosteroid medications reduce airway inflammation and can help prevent exacerbations or a sudden worsening of symptoms. These medications are useful for some people with COPD, specifically for those with frequent exacerbations, and are used as a dual-action therapy with bronchodilators.
Some medications combine bronchodilators and inhaled steroids to make it easier and simpler to take medication daily by cutting down on the number of separate inhalers to use as well as cutting cost for the patient.
For people who have a moderate or severe acute exacerbation, short courses of oral corticosteroids prevent further worsening of COPD. However, long-term use of these medications can have serious side effects, such as weight gain, diabetes, osteoporosis, cataracts and an increased risk of infection.
Another type of medication approved for people with severe emphysema and symptoms of chronic bronchitis is a phosphodiesterase-4 inhibitor. Your doctor may prescribe this drug to decrease airway inflammation and relax the airways. Common side effects include diarrhea and weight loss.
Respiratory infections, such as acute bronchitis, pneumonia and influenza, can aggravate your symptoms. Antibiotics help treat acute exacerbations, but they aren’t generally recommended for prevention.
Oxygen Therapy
 Oxygen therapy is used to improve oxygen levels, reduce damage and stress to vital organs and improve quality of life. Home oxygen can sometimes be prescribed if you have low blood oxygen levels.
Oxygen therapy is used to improve oxygen levels, reduce damage and stress to vital organs and improve quality of life. Home oxygen can sometimes be prescribed if you have low blood oxygen levels.
There are several devices to deliver oxygen to your lungs, including lightweight, portable units that you can take with you to run errands and get around town.
Some people with emphysema are prescribed to use oxygen only during activities or while sleeping. Others use oxygen all the time. Talk to your doctor about your needs and options.
 Surgery
Surgery
Surgical options can be very effective in improving lung function and in a select group of patients with severe emphysema. Your doctor will be able to advise if you are likely to benefit from surgery because, as with any type of surgery, there are risks involved. There are a number of procedures available to patients meeting strict selection criteria.
Lung transplantation is a very complex therapy, which can improve survival and quality of life, but also carries a high risk of complications, including the risk of dying. Transplantation is only suitable for people who have no other options for treatment and survival or for those with significantly impaired quality of life.
However, not everyone qualifies for lung transplantation and those who do are limited by donor organ availability.
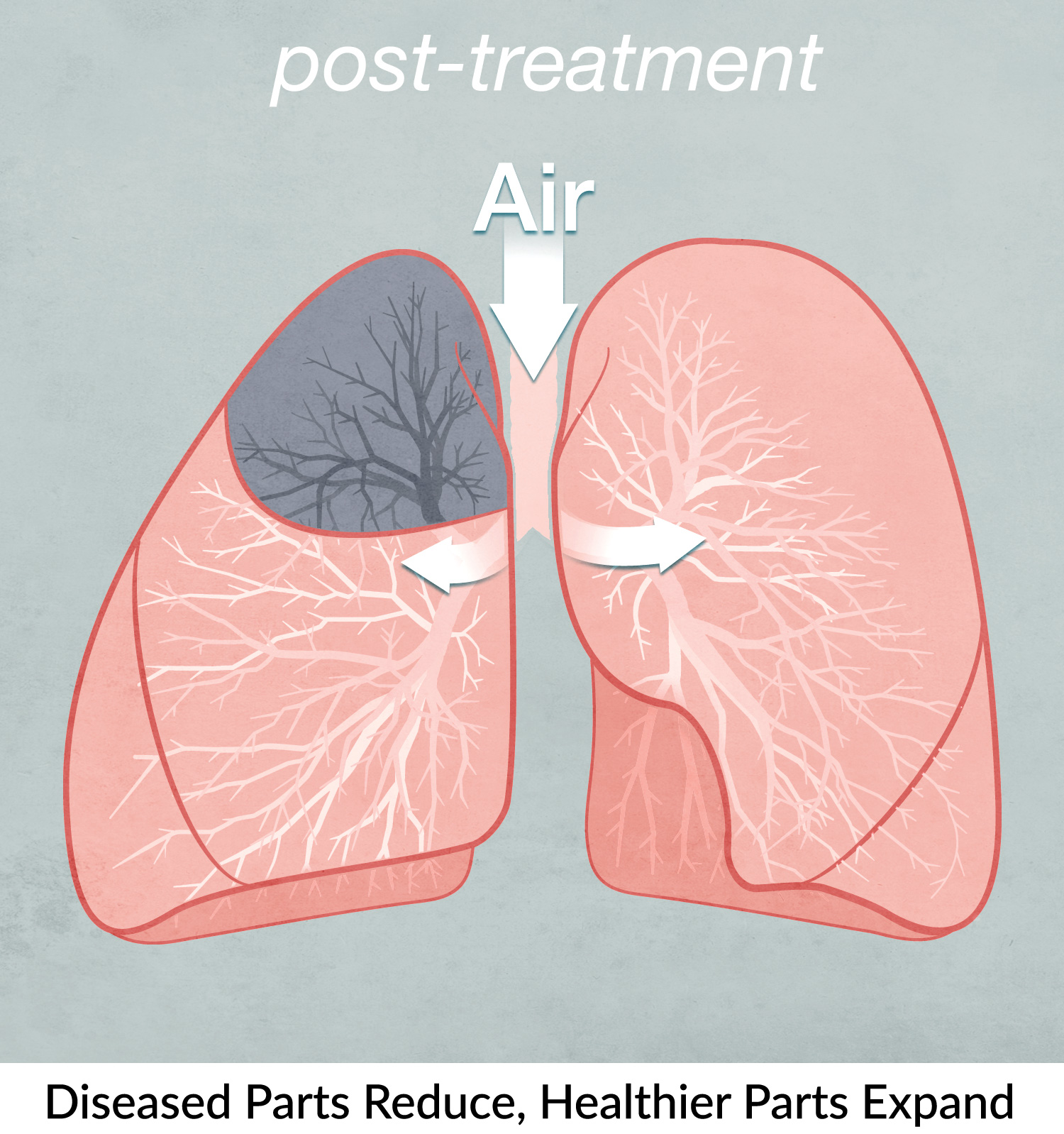
Lung volume reduction surgery (LVRS) is a surgical procedure that involves removal of the most diseased portions of the lungs. This allows healthier portions to expand thus improving lung mechanics and function.
Bullectomy is a surgical procedure to remove diseased air-filled spaces (bullae) that compress healthier parts of lungs. These diseased bullae do not contribute to gas exchange and therefore cannot enrich blood with oxygen.
Endobronchial Valve Therapy
While surgical options can be effective in improving lung function, there can be some serious risks involved. There are other minimally invasive treatment options available, such as endobronchial valve therapy, that can improve lung function significantly while avoiding the risk and recovery periods involved with more invasive surgery. Additionally, this treatment is fully reversible, meaning that the valves can be easily and safely removed if needed.
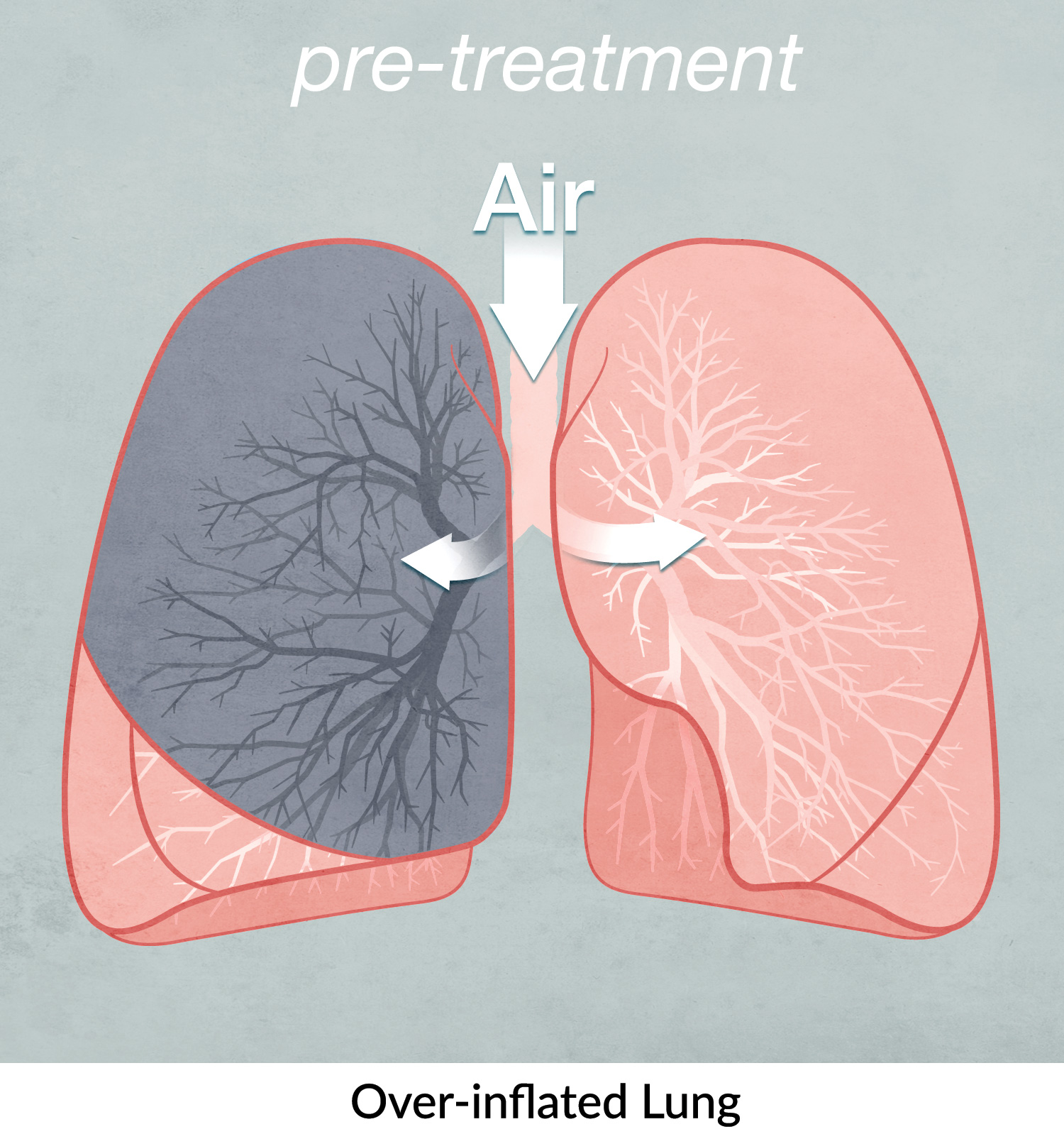
This procedure is not suitable for every patient with emphysema. It is important to understand that the procedure works by reducing the size of abnormally large lungs, so, unless the lungs are severely over-inflated to begin with, the treatment will not be effective.
The endobronchial valves are one-way devices that, once inserted into the airways, redirect air from the most diseased to the healthier parts of the lungs. Following the treatment, the volume of the treated part of the lung is gradually reduced, allowing healthier parts of the lung to expand and function more normally. This helps to reduce over-inflation, improve overall lung function and may relieve the symptoms of emphysema.
Once your doctor performs all the necessary tests and determines that you are a suitable candidate for this treatment, you will be admitted to hospital. The valves will be inserted during an endoscopic procedure, which means that surgery is not required. The procedure is usually performed under general anaesthetic through a device called a bronchoscope.
The entire procedure takes somewhere between 10 and 40 minutes. Generally, more than one valve will be placed in your lungs in order to block the most diseased part. Once implanted, the valves will stop any new air from entering that part of the lung while allowing trapped air and secretions to escape. Even though the valves are designed to stay in your lungs permanently, they can be easily removed if necessary.
After the procedure you will be closely monitored in hospital for a minimum of one night prior to going home.
During your hospital stay you may need to undergo a number of simple tests, including blood tests and chest x-rays to ensure your oxygen levels are within normal limits and also to rule out any complications.
Valve therapy is a minimally invasive procedure that is well tolerated by most patients, but is not without risks. Potential complications associated with bronchoscopy and/or valve placement include, but are not limited to, COPD exacerbation, infection, local airway swelling at the site of valve implantation, and pneumothorax (air leaking into the space between the lung and the chest wall).
You may start feeling the positive effect of the procedure very soon after, however, in some cases it may take up to a few months before the improvement becomes really noticeable. This can be due to a variety of reasons, including severity of emphysema prior to treatment, general state of your health and your exercise capacity, the amount and distribution of emphysema in the lungs and many others.
In the first 12 months following the procedure, your physician will monitor your progress on a regular basis. They may need to repeat your lung function tests, check your exercise tolerance and perform a high resolution scan of your lungs. Occasionally, a repeat bronchoscopy may be required to review the position of the valves in your airways.
Discuss this treatment option with your doctor. If you are a suitable candidate for this procedure, your doctor will be able to refer you to a physician specialising in this procedure. The specialist will ask you to undergo tests and investigations which will help them determine if this therapy will work for you.
Some of the most commonly used tests are listed below.
Lung function tests to assess the severity of your disease
Generally, only people with severe or moderately-severe emphysema are suitable for valve therapy.
This will help your doctor to determine how over-inflated your lungs are compared to normal and therefore to decide if this is the right treatment for you.
Chest x-ray to look at your heart and lungs
The x-ray will tell your doctor if the appearance of your lungs is consistent with emphysema
High Resolution Computed tomography (HRCT) of your chest to look at your lungs in greater detail
This test provides specific information about the presence and the amount of damage your lungs have sustained from emphysema and can help predict if the procedure would be successful.
Other endoscopic lung volume reduction therapies
Other techniques for endoscopic (non-surgical) lung volume reduction are also available or being developed. These include:
- Endobronchial coil procedure
- Bronchoscopic thermal vapour ablation
- Biological Lung Volume Reduction using lung sealants
